Question & Answer...
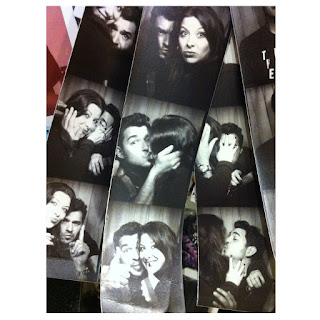
 A messed-up strip from one of my booths on route. I kind of like it... when the chemicals get old, they start to do weird, unpredictable things.
A messed-up strip from one of my booths on route. I kind of like it... when the chemicals get old, they start to do weird, unpredictable things.The following is a question / answer via email between me and my surgical team at UNMC. First, I just want to say, that the staff at UNMC is absolutely awesome about answering my questions in a punctual manner. I have also forwarded them my questions for Dr. Baum in Germany, but they were not sure about my questions for Dr. Baum, with respect to the 68-GA scan. This is not surprising because it’s not offered here in the US. Nevertheless, it seems as though some doctors here in the US are becoming aware of the importance of the 68-GA scan and PRRT. It’s probably not a silver bullet for everyone, but has had some great results –at least from what I have learned from other.
Letter to UNMC (To My Nurse Coordinator & Dr. Botha) From me:
Letter to UNMC (To My Nurse Coordinator & Dr. Botha) From me:
Dear (x),
I have my appointment with Dr. Baum, but have some additional questions I've been trying to have him answer. (He's apparently super busy...). Nevertheless, I'm confident that I want both the scan in Germany (since it seems reasonable) and the surgery with Dr. Botha. (The scan is NOT cheap). I had played with idea of skipping the scan in Bad Berka and heading right to Omaha, but figured that if it can help Jean, then lets go to Germany.
I do have some new questions / clarifications for you and/or Dr. Botha that have come up since my last visit:
1. Is the manual search for the primary tumor/s done prior to the work on the liver?
2. During a manual search for an unknown primary with the information we currently have (CT, MRI, Oscan), from your knowledge or experience, what are the statistics / percentages that this tumor may be found during the procedure?
3. If during the first operation, it was found that I was riddled with "Micro-Mets" (for instance, in the mesentery, or other areas), how would that be addressed? Would it halt the liver surgery? Or, would these mets be allowed to remain? How often do you see this situation (Once again, via knowledge and/or experience)?
4. If there is lymph node involvement, anywhere, would there be surgery in those areas? Would we even know if this were the case?
5. From my understanding, during the first surgery, we cut and/or reduce blood supply to the right lobe. If the left lobe does not show grow, the second stage of the surgery is cancelled. If this were to happen, eventually, new blood supplies to the right lobe will naturally grow and return supply to that part of the liver? From what I recall, the ties inserted are also designed to eventually dissolve? Is this all correct as I understand it?
6. If the 68-Ga scan were to reveal that my liver was worse than what we currently see (CT, MRI, Oscan), but the primary is identified, would we still surgically remove the primary? And if this were the case, would you suggest then debulking of the liver via spheres, RFA, etc., or, a more systemic approach such as PRRT?
REPLY #1
Anthony,
I'm going to forward your e-mail to Dr. Botha and hopefully he can answer all of the questions, but I will also give you my answers to the best of my knowledge.
I think Dr. Botha would look for the primary tumor before he starts the liver resection. Since it's more of a manual exploration I would assume that would come first and then Dr. Botha would address that tumor, if it's found, and the planned liver resections.
I don't know the percentage of time the unknown primary is found during the exploration.
I assume the plan during the surgery would be to remove as much tumor bulk as possible wherever it is found. So if there are tumors found in the mesentery that can be removed, or if there are suspicious lymph nodes that can be removed, I think Dr. Botha would remove those at the same time. I think if he were to find more disease in the liver than he felt he could safely remove that would halt the liver resection portion of the surgery.
I'll let Dr. Botha address your questions regarding the blood supply. Usually collateral blood vessels form over time when the main blood vessel is occluded, but I don't know about the material they use to occlude the vessel.
I know that it is advantageous to remove the primary tumor even if you cannot remove all of the tumors in the liver. However, the liver does need to have enough healthy tissue to tolerate a surgical procedure to resect the primary tumor without increasing the risks to the point where they outweigh the benefit of resecting the primary tumor. Again, I think Dr. Botha can better address this question.
I will review your questions with Dr. Botha and get his input. When I have that information I'll get in touch with you.
REPLY #2
Anthony,
I did review your questions with Dr. Botha and here are his responses.
He would look for the primary tumor before proceeding with the liver resection.
He states there is a 50-60% chance of finding the primary tumor during the exploration.
He did say that if during the surgery there are lots of mets found in the mesentery or other areas that he was not aware of before operating he would not proceed with the liver resection, but would resect the primary tumor (if it is found) and remove your gallbladder.
He would assess the lymph nodes and remove any suspicious nodes he could.
If the blood supply to the right lobe is occluded new blood vessels would grow. Dr. Botha says the material they use to occlude the vessel does not dissolve.
If the gallium scan reveals more liver tumors Dr. Botha would not proceed with debulking of those tumors, but if the primary tumor was identified he would proceed with resection of the primary. If the liver tumors are not resectable then either PRRT (with Dr. Baum in Germany) or liver transplantation would be discussed as treatment options.
Dr. Botha did not know the answers to the questions you had addressed to Dr. Baum. He did not have an answer regarding whether the gallium scan would give him a better road map to follow. I think the biggest benefit of the gallium scan would be possibly identifying tumors we haven't seen yet which might rule out resection as a treatment option and also possibly identifying the primary tumor site.
Hope this helps! Again, I think we are fine waiting to schedule the surgery until you have had the scan done in Germany.


Comments
Post a Comment